Kelly Shepard, RRT, AE-C grew up with asthma and hated every minute of it, never really understanding its full power. Through her trials and struggles, Shepard dedicated herself to learning everything she can about the lungs. Here is her story on how she became an RT.
Growing up, Shepard didn’t want to think of herself as “diseased” or different from her peers. When her friends started engaging in risky behaviors like cigarette smoking, she joined them.
It all came crashing down her 20th birthday.
“I planned a big party and invited my friends over to celebrate,” Shepard said. In anticipation of a long night she decided to take a nap and didn’t wake up until she heard the doorbell announcing their arrival.
She jumped up and answered the door, only to hear her friends cry out in alarm: “Oh my God, she’s blue!”
“Apparently, I had a significant bronchospasm during my sleep,” Shepard said. In her rush to open the door and get the party started she ignored her symptoms and failed to stop and take her albuterol.
“The boys carried me upstairs while someone called an ambulance,” she said. Her best friend set up her nebulizer — something she had learned to do as a result of the many sleepovers they had had over the years — and that’s the last thing Shepard remembers about that night.
I could die
She woke up a week later in the ICU at the Naval Hospital in Bremerton, WA. The hospitalization would last a total of four weeks, and Shepard realized, for the first time in her life, she could die from her asthma.
“My mother, a pharmacist, would later tell me that she kept that from me as she didn’t want me to panic during an asthma attack,” Shepard said.
Clearly, it was always a risk. As a child, Shepard experienced numerous trips to the ER for her asthma and multiple hospitalizations. Her doctors tried almost every asthma medication that came on the market, and prednisone was a mainstay of her care.
When Azmacort — one of the first inhaled medications for asthma — was introduced in the mid-1980s, she was prescribed four puffs, four times a day. But she eventually developed a tolerance and even it quit working.
Friendliest staff members
After encountering several RTs during her hospitalization, who Shepard says were the “friendliest of all the staff members,” and realizing her asthma wasn’t being managed appropriately, she decided to go to RT school and learn everything she could about the lungs.
“I felt like the more I knew about the lungs and my disease process, the better decisions I could make and be more involved in my care,” Shepard said.
Following her pharmacology course, she went to her doctor and asked to be placed on Flovent, Serevent, and albuterol MDIs.
He asked her why, and she explained that from her studies she had determined she had developed a tolerance to Azmacort, and since theophylline was mainly used in pediatric patients, she wanted to try these other options.
“Unable to explain why current therapies would be better than Serevent, he pulled out his prescription pad and gave me exactly what I asked for,” Shepard said.
She has not been back to the ER or had a hospitalization or exacerbation since — and oh yes, she quit smoking too.
Finding her niche
Shepard graduated from the RT program at Seattle Central Community College in 1996. Like many new grads, she wanted the big hospital experience and spent several years in that setting before getting a call that would change her career trajectory.
“I received a phone call offering me a job teaching pulmonary rehab,” she said. “My initial response was, I don’t even really know what that is or how to do it.”
After learning the hours would be a standard 9 a.m. to 5 p.m., Monday through Friday, though, she decided to apply. The rest, she says, is history.
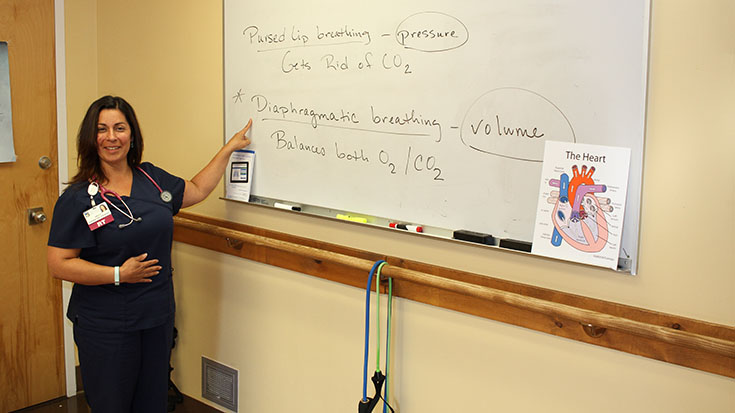
“I have been teaching PR since 2003 and really love working with people who are not acutely ill and are motivated to improve their quality of life and manage their disease to the best of their ability,” Shepard said.
Shepard says she enjoys the connections she is able to make with her patients and she shares her own respiratory challenges with them as they work to regain control of their own diseases.
She especially loves hearing the stories her older patients have to tell about everything they’ve experienced in their own lives.
“When I was a young mother, the ladies who came through my classes were a great resource on child rearing,” Shepard said. “I have received so much valuable advice.”
She’s often amazed at what these folks have lived through too.
“Two of the most beautiful souls I’ve had the fortune to know survived German concentration camps. Another patient flew on Air Force One with Lyndon B. Johnson. Yet another shared the same bus stop as Ted Bundy while growing up,” Shepard said. “The stories, the life experiences and adventures, that stuff just can’t be learned in school.”
Meant to be
Shepard truly believes her own life is a testament to the power of pulmonary rehabilitation.
“As a child, I asked God many times, ‘Why me? What did I do to deserve asthma?’” she said. “I now understand that I suffered to help others through their difficult time, to be the compassionate health care provider that would advocate for them to doctors, nurses, or insurance companies . . . I demonstrate to them how much power they have in their own healing process.”
Kelly Shepard is an RRT and AE-C at Peacehealth United General Medical Center in Sedro-Woolley, WA.