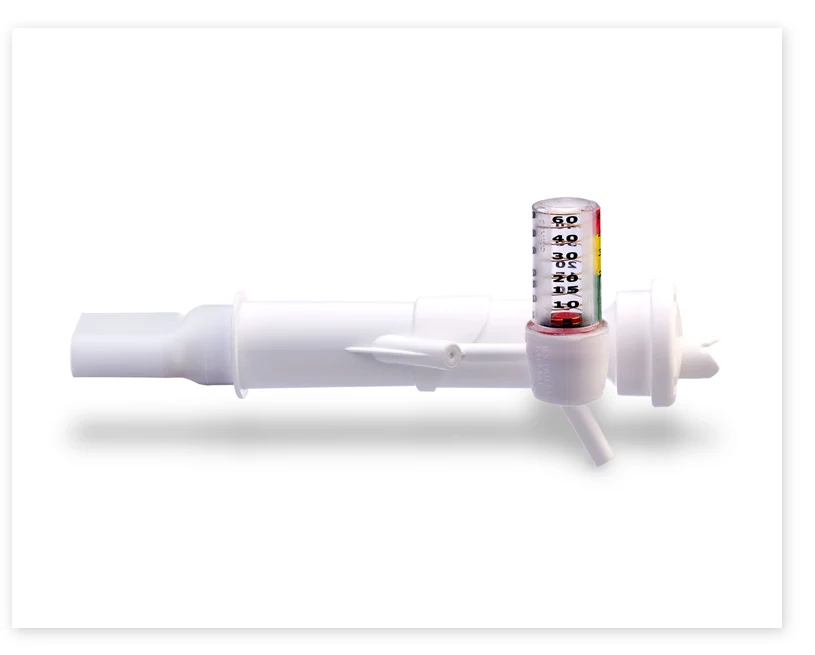
The VersaPAP® Device from Monaghan Medical
The VersaPAP® device was developed to provide clinicians with a single, simplified way to deliver positive airway pressure therapy. The integrated manometer provides immediate feedback and makes it easy to monitor for desired airway pressures.
All patients have the chance of developing some form of atelectasis post-surgically, but most will recover uneventfully.1 Atelectasis contributes to postoperative pulmonary complications which are common, serious and costly.1 The addition of Positive Airway Pressure (PAP) can help reduce or reverse partial or complete collapse of the lung.2 For patients who are at higher risk of developing atelectasis, incentive spirometry alone may not be enough.3


Hospital and DME Only:
Not available through retail pharmacies. For provider use only.
How It Works
PAP Therapy Is Helpful Because1
- Reduces Air Trapping
- Prevents Or Reverses Atelectasis
- Helps With Mucociliary Clearance
- Improves Delivery Of Inhaled Medications

ON INHALATION
- Increases the amount of air being inhaled
- Decreases the amount of work it takes to inhale
- Positive pressure helps stent airways open

ON EXHALATION
- Takes more effort against the flow of air
- Keeps the smaller airways from collapsing before the next breath in
How To Use

- Securely attach one end of the tubing to the device.
- Securely attach the other end of the tubing to the flow meter.
- Set the desired flow rate (starting at 5 L/min), slowly increasing to reach the desired expiratory airway pressure. Do not exceed a flow of 15 L/min.
- As the patient exhales through the device, verify that the manometer gauge is at the desired pressure range.
- Have the patient inhale and exhale for the prescribed amount of time.
References:
1RD Restrepo, Braverman J. Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis. Expert Rev Respir Med 2015;9(1):97-107.
2AARC Clinical Practice Guideline: Use of Positive Airway Pressure Adjuncts to Bronchial Hygiene Therapy. Respir Care 1993;38(5):516–521.
3RD Restrepo, Wettstein R, Wittnebel L, Tracy M. AARC Clinical Practice Guideline. Incentive Spirometry: 2011. Respir Care 2011;56(10):1600-1604.



