
Caring for the “whole” patient means many different things to many different people. But the bottom line for all is ensuring patients receive the compassionate care they need to heal. In our final 360 Degree Patient Care article, two RTs explain how they take their whole patient into account during the delivery of respiratory care.
The blind can lead
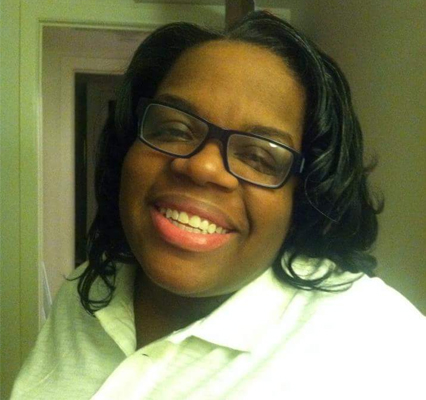
Gabrielle Davis, MPH, RRT, RRT-ACCS, RRT-NPS, is a COPD educator at St. Luke’s Hospital in Boise, ID, where she works to build relationships with her patients that she feels are essential to arming them with the tools they need to meet their self-management goals.
“Addressing the whole patient means addressing them and not their disease,” Davis said. “This means a COPD patient becomes a person with COPD.”
She puts her patients at ease by coming into their rooms with a small game of Scrabble or a deck of cards so they can bond over a game while they talk.
“Maybe we’ll chat while we play and I’ll learn something new about the patient affecting their ability,” she said. “Treating the patient as the leader of their own care versus a passive receiver of care can be very empowering for them.”
Letting the patient into her own life sometimes helps too. Davis recalls the special connection she made with one patient who was blind by sharing the experiences her own mother was having with her own impending blindness.
“When I entered the room, she was on a phone call that she immediately terminated when I walked in,” Davis said. “I told her where I was in proximity to her, introduced myself, and asked her if it was okay to provide the therapy that was scheduled.”
The woman thanked her and asked how she knew she was blind. Davis told her about her mom, and the patient immediately began offering her all the contacts she had to help with her mother’s approaching darkness.
“We talked for a half hour about living as a blind person,” Davis said. “When I prepared to leave she was thankful that I allowed her to help me, and treated her as an individual versus an ‘old blind lady.’”
Giant microbes!
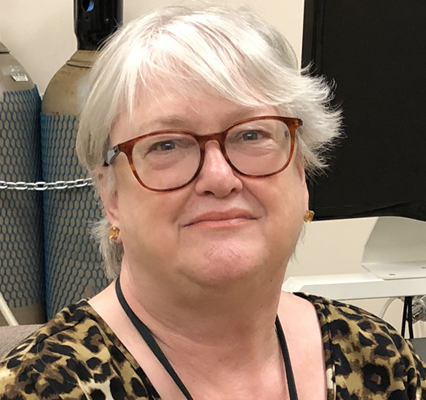
Of course, many RTs are so busy caring for the acute needs of their patients that time to address the whole patient is limited, at best.
Janet Cothrell, RRT, RPFT, who performs pulmonary function testing in the lab at the Seattle Cancer Care Alliance in Seattle, WA, shows there are still things an RT can do.
“If a patient comes to me and has MDIs with no spacers, I have arranged to give them spacers at no cost to them, and training and instruction sheets for use of said spacers,” Cothrell said.
She has acquired some hand-held nebulizers from a sales representative as well and gives them to patients on nebulizers, also with instructions for use and care.
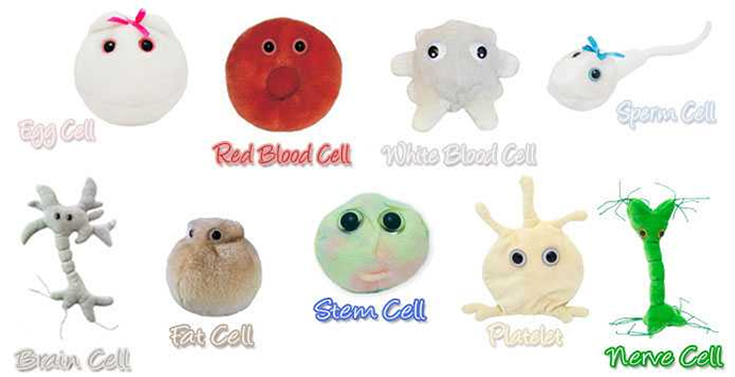
Pediatric patients who come to the lab for testing go home with ‘giant microbes’ — small stuffed toys depicting stem cells, red blood cells, white blood cells, and other ‘critters’ pertaining to their disease process.
It’s all part of a mission to show their patients they care.
“Our approach during testing is to be gentle and humorous — without letting the coaching suffer!” Cothrell said.